Dave DeBronkart ePatient Dave Part 1
ePatient Dave – Part I
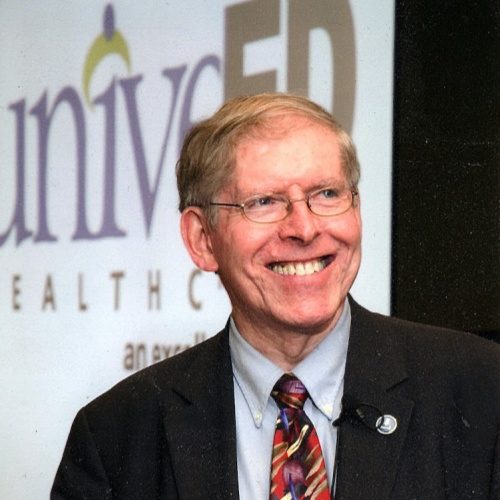
I’m honored to have Dave deBronkart on the podcast today. He is the original “e-Patient” and has a lot of stories and interesting projects to share with us today. As a matter of fact, so many interesting projects that we’re going to break this into a two-part discussion, so join me for our conversation with e-Patient Dave on Get Social Health.
Podcast Transcript
Announcer: 00:22 Welcome to Get Social Health, a conversation about social media and how it’s being used to help hospitals, social practices, healthcare practitioners and patients connect and engage via social media. Get Social Health, brings you conversations with professionals actively working in the field and provides real-life examples of healthcare social media in action. Here is your host, Janet Kennedy.
Janet: 00:48 Welcome to the Get Social Health podcast. What an honor for me to have Dave DeBronkart on the show today. He and I met through the Mayo Clinic Social Media Network and have run into each other a few times at healthcare conferences. It is such an honor to have him here. He’s known on the Internet as ePatient Dave. He’s the author of the highly rated “Let patients help patients” engagement handbook and he’s one of the world’s leading advocates for patient engagement. After beating stage four kidney cancer in 2007 he became a blogger, health policy advisor and international keynote speaker. Dave, welcome to the podcast.
Dave: 01:25 It’s an honor to be here. That’s what healthcare needs, so I’m really glad I’m quite, you do a good professional job of it.
Janet: 01:33 Thank you so much Dave, and I’m really thrilled to have you here. If anything, to give you an hour to sit down in a chair and just have a conversation because when I looked at your website and all your speaking engagements coming up, I was absolutely blown away with how active you are. You are talking to a lot of people these days.
Dave: 01:52 Well, do you know I can’t sit home and be an evangelist. You’ve got to carry it out into the field. And as it happens, through one of the strange quirks of the universe, when I accidentally found myself, it was actually 10 years ago this month, that I found myself on the front page of the Boston Globe because of a blog post I’d written. People started asking me to give speeches on the topic and I had learned how to do that when I worked in marketing. The last thing I ever would have expected coming out of cancer is that it would turn me into an international keynote speaker.
Janet: 02:26 I love that. I love that you felt that this is a mission worth all of your time, that you really wanted to commit to that. I know that we’re going to gloss over your early story because I think a lot of people know who you are, but what you represent an almost more than any other patients we’ve spoken with is that you’re a mature individual and you have a length of view that is longer than many of my guests. A lot of ePatients who are involved and engage these days tend to be in there like twenties and because they have always felt that social and digital was a way to tell their stories. You and I represent more of the boomer generation.
Dave: 03:07 Uh, we’re not so forthcoming.
Janet: 03:09 I’d love to get your perspective on this 2009 – 10 years ago when people first started you to speak as an engaged patient and an empowered patient. What’s happened since 2009 to today?
Dave: 03:23 Well, you know, I’ve just been reflecting on this because 12 years I got the diagnosis to nearly died, but God cured within a year. That was 2007 in some speeches. Now I customize every speech for the audience, depending on what they’re up to. Sometimes the best message is if you live long enough, things really change. And what’s important about that is people tend to achieve a certain level of seniority or accomplishment in their profession, whatever it may be. And they feel like, dude, I got this, I’m good at this. And then 10 years go by and all of a sudden what was important before isn’t important anymore. And you’ve got youngsters nipping at your heels and you got to think it all out again. So consider in the middle of my treatment, Apple introduced a product called the iPhone. You know, and you think that the world might have changed a bit since then.
Dave: 04:20 So, well, and that’s a, you know, apps and everything. And this is why in my career in business, I was involved in quality improvement projects, countless meetings over the years with different companies about rethinking how we go about doing things, what are our customer’s priorities and so on. So I naturally, when people started asking me to talk about how care, particularly patient engagement, I looked at it through that Lens. So what has changed in 10 years, 12 years and years since the front page article is, I’ve learned a lot more about what’s changed in the industry as a whole. A lot of people have been trying to do patient engagement, patient empowerment, and a whole lot of people have been pushing back. But it turns out that a lot of big reason for that, you can’t do patient empowerment and engagement with any sort of completeness unless the patient has access to the medical records. And there has been feeble lip service in the past because the technology didn’t support it. But you know, the biggest change in what it looks like if you look out to the horizon is the technology is coming along and the culture is finally coming along 10 years later to make it possible for us to get all of our information.
Janet: 05:50 And that is really the foundation of helping patients knowing and participate in their health journeys, right? They have to have access to what the doctors are saying about them and what the doctors are cataloging about them, correct?
Dave: 06:04 Well, in general, yes. Now, not everybody one flat. All right. Because the whole principle of patients that are care is that people are different and you can’t treat everybody the same. It’s, I’ve found it’s useful to point out to people, especially if it’s an audience that is in the younger parents category. Like my daughter is, I have a five-year-old granddaughter, excuse me, 5.8 years old.
Dave: 06:32 Her mother is a science teacher, she is 5.8 years old. Anyway, people who are recent parents, no, you can’t treat all little kids the same. Some of them wanted to take things slow and easy, somewhat excitement and so on. Some patients during my illness, the nurse practitioner over men, that’s just my case said that she used to work in pediatric oncology and sometimes the patient couldn’t articulate what was important to them. First of all, not everybody cares about seeing what’s in their health records. My parents are polar opposites on that. My father just said let them do their job. It’s my mom is just on top of everything checking to make sure they’ve got her allergies and medications right and everything. My point is it is perverse. Take, keep people like patient in the dark about something and then go around saying they wouldn’t understand. They don’t know anything about this.
Dave: 07:33 You see my point? It’s exactly, there’s so many parallels between the ePatient movement than the women’s movement. When I was a little kid, people were always making jokes on TV about women drivers. Well, women were not experienced drivers in the early 1950s generally, you know, the remedy was not to keep people in the dark. The remedy was to get them involved and make them experience. And that’s my point with patient access to the medical record. It’s really is unfair. It’s an unfair burden to expect the providers to be on top of everything because there’s so much stuff in a chart, it really is much better to let patients help.
Janet: 08:18 So are you saying that, and I agree with you totally, I love your analogy too. Hey, nobody’s going to get to be a better driver unless they get to drive. No one is going to appreciate their health records unless they see their health records. But are you saying that this is literally just having access to the EHR, whether you choose to engage with the electronic health record or not, is the point or is there a deeper level of information you think that patients need?
Dave: 08:42 That’s an excellent question. I have a lot of conversations on this subject and that’s a razor-sharp question. My goal is not to make people do anything a particular way. It’s to help healthcare achieve its potential. I am deeply grateful to the highly skilled, trained, educated doctors, nurses, assistants, everyone who took good care of me when I was dying and in my business troubleshooting mindset. When I hear all the stories about medical errors or somebody didn’t know about a side effect or just there are so many ways that the flood of information out there might not get to the point of need at the moment of need and what I want. First, we troubleshoot. We say, wow, there is too much information for anybody to know everything, so now what can we do? Some people say, well, it’s the doctor’s job to know everything.
Dave: 09:50 Well, well, I know you and I were immersed in this, but the general public has not had this OMG moment of realization yet. It’s funny if the ePatient expects the doctor to know everything, it’s a recipe for mischief. The same is true if the doctor expects to be treated like they know everything, you know? And that’s so this is why this is a culture change, you know, in the women’s movement. Well, what it taught to change mindsets and we thought we had it solved, but oh boy seems that it’s an ongoing project. What it took to change mindsets was not just changing men’s minds, but women’s minds. Also long ago, early in my career, I had a woman who worked for me, literally said she couldn’t do something. She said I’m just a girl. Like you see, you are a level three employee, which is a high level in a technical profession. Yeah. So it is a culture change.
Janet: 10:53 All right, so what are the things you talk about as, as a goal or a priority on a professional side is that you really want social change and I think that’s really the point that you were just making. But how do you envision social change helping healthcare and making healthcare easier for patients?
Dave: 11:14 Well, you know, just this morning, a patient blogger named Aaron Gilmer, Gilmer health law is her Twitter handle, posted something magnificent. One of the best achievements, I think in patient engagement with empowerment that I’ve ever seen. She has, an extreme mix of psychological and trauma and medical conditions and so on. She created two documents that are now in her chart that express what heart concerns are about being taken care of, how past traumas affect various things, what they should know, what she does in order to deal with it. And here’s how I express my worry if I’ve been triggered. And so on. The first hospitals she gave it to, they looked at it and canceled her surgery. They basically said, get outta here. And she didn’t bring it up again. She has a great blog post about it. We can link to it in the show notes.
Dave: 12:18 She didn’t bring it up again. And then several years later, just recently she got additional care that happened to be in part of the same system. They ran across this and they said, thank you so much. And they have been using what she had expressed. They’ve been using those methods of talking with her and are you okay with this? And so on. See that’s social change. In the old view, the doctor knows everything and those what you’re supposed to get economically. This can be a major issue because in US healthcare, so much of what care providers are allowed to do is tied to reimbursement issues and there can be financial pressures. It really takes commitment as a caring profession to overcome that and in the new view, it really is important what matters to the individual patient and people are committed to care as a separate issue from the science that’s being administered to the sick person.
Janet: 13:27 Alright Dave, I’m having an epiphany here and I don’t know why this never occurred to me. Although I will say I have the benefit of being a generally healthy person. I’ve never really had any serious health issues and a visit to the doctor will solve my problem. So I’m very, very fortunate in that regard. However, it never occurred to me that as a patient do I even have the right to add things to my own file and why we should allow patients to submit a patient statement. That kind of sets it up, especially if you’re going from physician to physician, you’d have a complicated thing. Wouldn’t you rather be able to say, here’s my – just what Aaron Gilmer did – here’s my story, here’s my whatever. So that as you get from a specialist, to specialist, to specialist, they actually read just a paragraph about who you are as a person, not who you are as a series of medical diagnoses.
Dave: 14:16 Absolutely. And I imagine that in your work, I mean will you manage client relationships and your business? You need to understand what’s important for them, right? You walk in, if you get on a first phone call with everyone and you just feel out the same thing you said to the last 12 people and here you go. Like it or not, I’m going to give you my off the shelf solution. Well, you don’t like that. What’s wrong with you? Right? You would think that the doctor knows what to do in every visit. But in today’s world, you’ve got to ask yourself what, so what’s the difference between what you do in service to your clients and what a physicians, MD, nurse practitioner – by the way, it was a nurse practitioner who first told Erin that he found that in her chart and he was so grateful for it.
Dave: 15:10 That’s a whole separate discussion of how nurse practitioners generally have more of a cultural license, so to speak. Figuratively speaking, to just plain be caring professionals. What are the cultural reasons why we – in healthcare – we wouldn’t start with finding out what’s important. I mean, my doctor, the famous doctor Danny Sands, he was the one who in 2007 when it turns out I was dying. He, was the one who you have a good patient community and he didn’t say stay off the Internet. He showed me where to go on the Internet.
Janet: 15:52 Oh wow. He’s unusual.
Dave: 15:52 Well that’s, that’s modern. That’s modern today. He wears, I just saw on my last clinical visit with him, he has a button on his wife coat that says what matters to you with a question mark, what matters to you? Because you know, you prescribed somebody, okay, you got to eat better.
Dave: 16:17 You gotta do this, you’ve got to do that. That’s all external shut up and do what I tell you. Unless it is grounded in me one thing, some form of a better life, to know that somebody really would love to live to see their grandchildren get married versus my bucket list has one big item. It’s a month in Hawaii. You know? Then any recommendation for exercise or behavior change or anything. And that’s, that’s the point these days. We have so many options, treatment options and so on. All proper respect and appreciation to physicians who in today’s economic environment, we’ll take that extra time because they don’t get paid any more for being that kind of a good physician.
Janet: 17:10 Hmm. Okay. Dave, I want to ask your perspective on something. The world I’m in where, again, as a fortunately healthy person and in my podcast, the work I do tends to be with startups, with new companies, with digital health folks, with young people who are inventing apps and it’s a very exciting world. However, I know you’ve spoken to physicians and healthcare practitioners in the hospital environment and one of the things that I feel is happening and I’m looking to you for clarification or validation is what’s up with the medical schools? Are they focusing on integrating some of these new ideas and changes or are still training physicians the same way they always did? Therefore, we’re just going to have one more generation of folks who want to say do as I say,
Dave: 17:57 Well, surprise, surprise. There’s a spectrum. Whoever would have thought that there would be, we know social change takes generations, right? The conventional wisdom that I’ve heard physicians express to each other is, you don’t want to be the first to do something new and you don’t want to be the last, just stay in the middle of the pack. Now, surprise, surprise. That turns out to also be exactly how the curve in high tech innovation; there’s to this curve where you have the early adopters, the innovators, then you have the early majority and so on, and then the laggards are the last ones to get into it. Some medical schools are primarily interested in preserving their reputation and their position. They want to do a good job of doing what’s well accepted. I don’t necessarily fault that. I do think it’s a good way to guarantee that you will never be in leadership.
Dave: 19:01 You know, you may be leadership and reputation, but you’ll never be leadership and turning out of the next generation of innovative, smartest, best future doctors. Others though new medical schools that come along and the best example that I know of is the Dell medical school at the University of Texas. That has just opened recently. An example of how they’re willing to conspicuously differ because there is this thing that some of us learned in high school, high school biology, the Krebs cycle, how energy gets generated. And I don’t remember a thing about it. And the important thing is it’s always been something that doctors have to master in order to become an MB and then they never ever use it. So why is it taught and why is it so important? Some people think it’s just to be obnoxious and make it difficult to get over that hump.
Dave: 20:01 Anyway, Dell medical school’s conspicuously said, we’re not teaching the Krebs Cycle. We’ve got better things to do with our time. And similarly there is a great social penalty within the medical community or going after something that is not well established with a larger body of published literature about it. So to get deeply into patient engagement today is risky in that context. People will say, where’s the evidence for that? And that’s good because once upon a time, you know, just within the last 50 years, it was discovered that doctors were doing a lot of things despite the that it doesn’t work.
Dave: 20:50 And that’s a whole separate subject. My point is it takes genuine vision and leadership to see that something is the new path forward, even if the literature doesn’t exist for it. And some schools are beginning to do that, but not enough. I have begun lecturing to some medical schools. Just as one final hint of that. I opened an email late 2014 and it was an invitation from the Mayo Clinic, from their chief residents to be there visiting professor in internal medicine in 2015 despite the absence of any curriculum or anything of the sort. So I went to, we talked a lot about the future of the role of the patient.
Janet: 21:41 Well, I love working with the team at Mayo Clinic. Now I haven’t been on the clinical side, obviously I’ve been on the social media side, but the embracing new ideas and at least let’s look at everything and what is it’s potential impact is just a phenomenal philosophy that you don’t turn your back on it till it’s, you know, so proved, it’s carved in stone. Dave, you’ve teamed up with probably one of the most well known medical futurists and medical device testers in the world. Dr Bertalan Mesko. What did you do with him and what is the digital health manifesto?
Dave: 22:16 Well, it’s an ongoing thing. You know, and it’s funny because this just freaks me out. One of the things that changed, I said if you live long enough, things change. Well, one thing that’s happened is I am 12 years older than I was 12 years ago. And that means for instance that my daughter who was just getting out of college when I was sick is now a mid-career science teacher. And I can’t believe this, but Bersi is younger than my daughter. And so there we are having these conversations and he’s showing me all his digital gadgets and we actually both spoke at a conference. A company had a, an important user group meeting in Chicago a few months ago. We both spoke one after the other and he and I both are thinking in terms of what could we be achieving and what’s holding it back. And we see, especially on LinkedIn, LinkedIn is a wonderful place for making connections and so on. But you’ll also see in the same way that Twitter became a sort of a festering swamp of rumors and illusions. On LinkedIn, you can see investor type people, Silicon Valley type people getting frothed up about a wrong concept and just the fact that other people are getting excited about it makes it seem like this must be the right thing. So we decided together to publish this manifesto saying, Whoa, step back you guys. Just because something is an amazing new technology. I like to think of it in terms of the Pharma concept, pharmacological concept of what’s the mechanism of action by which this new gadget is going to improve anything. You know, so many silicon valley inventions, as well, meaning as they were, turn out to not make any difference or they make a difference, but they don’t get commercial uptake and they die.
Dave: 24:26 So we wanted to point out, here are the principles that you need to think about if you want to understand what’s happening with digital health, because believe us, something real is happening. I used gadgets, for instance, to overcome prediabetes a few years ago, and everybody, I’m over 60 I’m well over 60 and a bunch of people said, look, people over 60 aren’t going to ever change their behavior. It’s a lost cause. Those people are ignorant. All right? So we said principals, it’s a cultural transformation, not a technological revolution. All right? It’s about behavior change. It’s not about – see when I, when I got this prediabetes diagnosis, I went out and bought a Garmin wristband and I collected lots of data about my activity and my weight went up. Well. So here’s the thing. Information enables behavior change, but it doesn’t cause it. What produced weight loss for me and a victory was that I got into the YMCA’s diabetes prevention program, which is a behavior change program. Okay? So it’s not about having the technology. What’s important about that from a business sense for a couple of years, cynics – so you have the enthusiasts on LinkedIn who are blabbing about how exciting this innovation is and then you always have the wave of cynics who come along and say, yeah, you know, where you go ahead and search, buy a Fitbit. You know what you find? You find ads for used ones that have been discarded on eBay. Those are stupid people who say that because somebody buys the Fitbit and they expect it to reverse their prediabetes stupid. And when I say stupid, I mean uninformed, right? It’s okay for me. If somebody is uninformed and they admit it, which I do a lot. But if they are uninformed and they go around with their chest puffed out acting like they’re smart, that’s ignorant.
Janet: 26:36 Well I know there’s been conversations about around ADHD; that ADHD with med and no behavior modification, you’re better off not taking the meds at all. So you have to understand how the medication or how the issue is impacting your body and be able to take action as well as work with the med.
Dave: 26:57 Well. And so now, to switch back to Erin Gilmer’s perspective, because all this stuff is interrelated as everything cultural is. One of the first things I did online before the Internet was back on Compuserve. I started out being a discussion leader in desktop publishing and then I became one of the forum managers on the ADD forum back when it was called ADD. And one of the things you found there was that when the people who have the problem, and I still pitch this in speeches today for certain audiences, when the people who have the problem get the ability to express themselves and choose among options, one of the things you find is they may pursue different objectives than the therapists or being told to follow what’s in the published literature, so as just one of many examples. We had one guy – and this was 1994 was when ADD was brand new – we had one guy who was a travel agent back in the days of travel agents. Did I mention that things change? And he was getting occupational therapy so he could tolerate sitting at his desk and the other patients in the community said, dude, get a job you enjoy, and he ended up becoming a UPS driver, which was a great job for our hyperactive person. Drive, drive, drive and run to the door, drive, drive, drive, run to the door at Christmas time you get bonuses for productivity. That’s rethinking the issue. Anyway, my point is this really is like a seismic shift because if you shift to where you’re giving the person who has the problem, permission and information and tools, what they come up with may be different than what was on offer at the hospital. That can be bad news for the hospital, but since the hospital only exists to improve health in the community, it’s good for society.
Janet: 29:13 No, that’s an excellent point, Dave, and I definitely think it’s one that hospitals need to hear just because you have a perspective that this, you’re going to do this program, you’re going to initiate this special effort or this patient initiative. It doesn’t mean that the results are expected and you have to be willing to be flexible and learn from what you’re doing as well as the patient learning from it.
Dave: 29:39 Well, and what I really hope, I don’t want to sound like I’m rejecting doctors. That’s the last thing. When I was sick, I did not reject doctors and go read up on herbal remedies. That might work. I went to the doctor, I still go to the doctor, but my doctor welcomes all of my doctors. Welcome me wanting to learn more and ask questions. That’s the point. And now you want to know what’s really ironic. So I have all these different apps. I have a wifi bathroom scale, I have my diet tracker or I’m counting fat grams, steps, and all of that stuff. My doctor can’t see that data because there’s big fancy hospital computer doesn’t have an interface. So now we’re in a world where all of a sudden I have access to a ton of data that he doesn’t have. That is an inversion.
Janet: 30:40 And so we have to figure out how to get those two things married up.
Dave: 30:43 Perhaps. It may be that he can do his job as well as he needs to without seeing all my data. But we were just approaching, there’s a new it technology called FHIR – F H I R – which is just really maturing now after six or seven years of software development that will, for the first time, let people develop products that blend the hospital information, hospitals, plural. And my information from my devices. So there is a world coming where we can truly be partners in the same way that my tax accountant and I can both look at my Quickbooks data. Why as medicine not figured out that that’s the best way. Now my tax accountant can coach me to stop doing this. See this over here? That number’s too big. Why can’t my doctor do that? My whole thing is helping healthcare achieve the available potential.
Janet: 31:47 Oh, that’s excellent.
Announcer: 31:49 You’ve been listening to the Get Social Health podcast. The show notes are located @getsocialhealth.com to join our healthcare social media journey, follow @getsocialhealth on Twitter and start a conversation.
Janet: 32:04 I hope you enjoyed today’s podcast with Dave deBronkart. We’re going to be talking about some of the projects he’s working on and some exciting new things happening in his life in the next episode. So make sure you tune in for part two of our conversation with e-Patient Dave.
Find Dave online:
LinkedIn profile: http://LinkedIn.com/in/ePatientDave
Twitter: @ePatientDave
Podcast: Play in new window | Download